A ‘mysterious’ heel bump (Part 2)
Thanks for reading my latest article on ‘Haglund’s deformity’
Let me try to demystify one type of heel pain known simply as the pump bump. Patients often ask how does a heel bump it arise and what we can do about my heel bump?
Vaishya (2016) calls it a ‘common but mysterious condition’ in his paper . The reader needs to be aware that heel bump is a simplification and has some complex names. There are plenty of reasons for heel pain and this is one.
The retro calcaneal exostosis or Haglund’s deformity sound mysterious. Haglund as a name for a heel condition was so called after the man who described the problem in 1927.
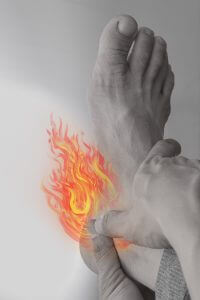
I have this heel condition myself. My problem has been with me for thirty years. It was not until I was in my late forties that I experienced problems. My main concern was whilst driving, then latterly when wearing some designs of shoes. This has made me more aware of the design of my shoe. Pressure from the floor of the car stung my foot like crazy because my heel rubbed the skin while the foot was against the floor of the car. There were times when some shoes could rub the skin forming a blister.
What is it?
When studying to become a podiatrist, we called these heel bumps an exostosis or simply Haglund’s. The condition is not a disease but a deformity of the back of the heel bone (calcaneus). The term syndrome suggests that there is more than one condition.
Those who read my articles regularly know that I try to keep descriptions as simple as possible. Here is Vaishya’s complicated reasoning about the condition but I will explain what all the jargon is after his paragraph.
Haglund’s deformity is an abnormality of the posterosuperior part of the calcaneus, where there is a bony enlargement at the attachment of the Achilles tendon. The adjoining soft tissues can get irritated when this bony lump rubs against rigid shoes. It often leads to retrocalcaneal bursitis, calcaneal tendon bursitis, and thickening and inflammation of the calcaneal tendon. This combination of pathology is known as Haglund’s syndrome. Inflammation of the different parts of soft tissue in the area can lead to an isolated condition; however, the treatment options are different in these conditions, and so they should be differentiated.
We now know the heel has a protrusion but let’s keep it simple. ‘Posterosuperior‘ is an anatomical position. The back of the heel! What about the tendon. Most people only have the minor form of bump. However, in a few people the bump becomes larger. If the extent of the bone extend across the heel, where the big tendon of the calf is anchored, then part of the tendon can also be involved.
It can do so in three ways.
The tendon can be damaged, or the skin can form a spongy fluid filled sac called a bursa. Where the deep tendon sac becomes inflamed the condition can deteriorate. The skin surface can form a blister.Blisters are caused through frictional pressure. In rarer cases of heel pain the tendon is also involved and the protective cushions or bursal sacs add to the pain together with unhelpful swelling. Bursa Sac. The UK site shown on clicking over the bursa sac is shown for the diagram. The content has not been validated by ConsultingFootPain. This is an independent practice orthopaedic site.
How is it caused?
As to the cause, Vaishya saysit is mostly an idiopathic condition, but several contributory factors like over-practice in runners, tight or poorly fitting shoes, or altered biomechanics of foot joints because of the dealigned subtalar joint may play a role
Idiopathic means we don’t know or that the condition occurs without a clear reason. Poor fitting of shoes is often due to the fact that the shoe does not suit the foot with a heel bump.
Runners only experience this problem because they increase the process of friction during running. This does not happen to runners only.
Altered Biomechanics
While this label makes sense to podiatrists to the average man on the street the word is just gobbledegook! Throw in the an anatomical label such as subtalar joint (Fig.2) and this might confuse most people. This just means the lower half of the ankle joint.
Let me describe the process in simple language.
The skin rubs against the shoe but deeper pressure changes the thickness of the bone lining (periosteum). The periosteum adapts by laying down more bone. This arises where pressure and stress are greatest. For those with a fascination for the biology, this video makes for good education. The process of bone being adapted is well known and is called Wolff’s law. But what starts it off. Back to that word BIO-mechanics.
Mechanics
Mechanics implies the way things work or function according to physical principles. The foot is a wonder of mechanics. As it is living and biological we call the movement and function ‘bio-mechanics’. As the heel contacts the ground it rotates sideways making contact with the inside lining of the shoe. This movement is called eversion and inversion so in reality tipping motions. This movement happens at one key joint. This is the subtalar joint. The forty-eight second video will be helpful to understand ankle movements. You can tell if this is a long standing problem because the bone wears a small hole in the lining of the shoe.
If there is too much movement between the foot and the shoe then the skin builds up friction (Fig.1). The foot moves in other directions, such as up and down at the true ankle joint (Fig. 2). Compression of the skin and deeper parts distort and set up shearing. Shearing forces are made from both friction (C) and compression (D) and create deep damage.
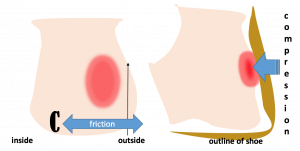
Figure 1 two views of the heel (left back, right side view). Area of skin stress shown in red.
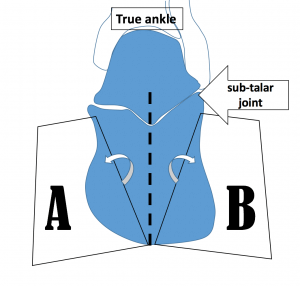
Figure 2. The subtalar joint is shown and pivots sideways toward A (eversion) or toward B (inversion) during walking. If the movement across both positions increases, excessively then the deeper fictional forces causes shearing across the soft parts which become inflamed.
What can we do about your heel bump?

The first consideration is to manage any broken skin (acute injury). Prevention is better and so awareness of the shoe, your foot deformity and the surrounding terrain becomes a useful formula.
Haglund’s ‘syndrome’ suggests (1) the skin might be irritated, or that (2) a deep bursa has become inflamed. This might have developed with some (3) tendon involvement. All three components might be present but often it is only the bump that causes soreness. If it is simply the communal garden swelling, conservative management can be achieved by altering the heel height in shoe wear or using some type of local protection.
The aim of any self-help management is to prevent blistering from arising or the skin breaking and forming a ‘wound’. For anyone with neuropathy DO NOTE that damage can arise without any immediate knowledge. Naturally this has greater concern for patients with diabetes who suffer from numbness or neuropathy.

Gel sleeve is made from a thin elastic stocking with a thin spongy pad formed into the sock as shown.
Acute
Direct skin pressure can be alleviated by using a blister patch, but these should really be used when acutely inflamed or where the skin has broken. Blister patches are sold in local pharmacies and chemist outlets.
A wound dressing will help absorb any leaking fluid to prevent infection. Change this regularly until the any fluid leakage has stopped. Leave open to air at night providing that the foot does not stick to the sheets. Place a soft pillow or reposition yourself at night at the back of the leg (above the heel) to take pressure away from the raw skin.
Use a fresh dry dressing during the day. Avoid any further pressure and reduced the use of dressings unless necessary. Footwear such as flip flops, sandals or Crocs will help limit skin pressure while the skin mends. Pain medication is not required unless the level of pain if high, in which case if this is sustained for more than 2 days seek help from a professional. Normal pain medicines for headaches work.
Try not to burst the roof of any blister unless this has become so large it will burst with footwear pressure anyway. To burst a blister you must use a clean technique. Use a standard antiseptic dressing is better than recommendations to use vaseline and certainly preferred to antibiotic creams. As a rule of thumb, ointments should not be used on open wounds. There are always exceptions.
Prevention
The use of a siliconised gel sleeve, as shown in the picture above is highly effective and I have used this for walks when shoes that I know cause me problems despite fitting well enough. A felt pad cut out stuck to the inside of the shoe is helpful. This is often called a donut pad and similar to the bunion pad I have demonstrated as part of my self help videos.
New blister patch

PelliTec(R) is explained in this exploded diagram
Adhering anything stick to the foot can damage the skin.
One of the problems with sticking anything to the skin is that in a short time the skin will become damaged. A recent pad that I have trialed is the ‘Pellitec’ blister patch. This can be stuck to the shoe in much the same way as felt can be applied. The pad is small and takes up little room, but it must be placed correctly. Measuring around 4.5cm in diameter it should not be stuck to the skin.
Mike McColgan has written about this in a recent article for ConsultingFootPain.

Initially I had difficulty fitting the pad inside the heel of my walking boot. The area pressed and the foam layer flattened. After a little trial and error, the pad worked and has stayed in place and curiously has not flattened out after 6 weeks. As my walking increased during the period of Lockdown in March-May 2020 I must have walked a good 50 miles with my new blister pad and had no problem. My trusty boots had just become even more comfortable. To date I have eradicated all shoes from causing pressure to my heel.
Surgery
Most of the formal professional sites that I have recommended all say something about surgery. This is not always a successful operation for large bumps. Smaller bumps, like my own, would work well enough if operated on. Recovery time is longer than you may realise; no less than 6 weeks and sometimes longer. Surgery is not for the faint hearted and the inconvenience is more to do with inconvenience than any lack of success. The usual risks exist but this is where most sites do offer detailed information.
As Vaishya suggests, ‘surgical excision of the bony exostoses of the calcaneum is only required in resistant cases.’ His further advice is also valid.
‘Inflammation of the different parts of soft tissue in the area can lead to an isolated condition; however, the treatment options are different in these conditions, and so they should be differentiated.’
This condition can affect one or both heels. A history of arthritic conditions such as gout, rheumatoid arthritis, or seronegative spondyloarthropathies should be considered (Vaishya).
ConsultingFoot Pain says best sources are
ACFS and FootEducation

Fig.3 Courtesy College of Podiatry (open access) shows callus formation. The bump is toward the outside of the foot as in Fig. 1
The American College of Foot surgeons (good ***) has produced a useful overall impression as does my usual site FootEducation (good***) which also uses the term ‘pump bump’. The British Foot and Ankle Society (poor*) does not talk about this condition within its brief discussion around heel pain while the College of podiatry (Useful**) make a brief statement (see box) and considers surgery as the other links.
| Some people develop bumps on the back of the heel, often referred to as “pump bumps”. These are often a combination of local skin thickening, bursa and enlargement of the heel bone. This condition requires very careful investigation to determine the extent of the bump and whether there is any bone formed within the tendon. Depending on where the bump is and what structures are involved, treatment can sometimes be very difficult. Surgery is often associated with prolonged recovery and persistent swelling.College of Podiatry |
Vaishya,R, Agarwal,AK, Azizi,AT, Vijay,V. Haglund’s Syndrome: A Commonly Seen Mysterious Condition. Oct; 8(10): e820. Published online 2016 Oct 7. doi: 10.7759/cureus.820